Breadcrumbs
Case of the Month: April 2024
Clinical history
A 22-year-old woman presents with recurrent episodes of diarrhea, crampy abdominal pain, and slight fever over the last 2 years. At first the episodes, which usually last 1 or 2 weeks, were several months apart, but recently they have occurred more frequently. Other symptoms have included mild joint pain and sometimes red skin lesions. On at least one occasion, her stool has been guaiac-positive, indicating the presence of occult blood. A colonoscopy was performed, which showed patchy sharply delineated areas with thickening of the bowel wall and mucosal ulceration. Areas adjacent to these lesions appear normal. Several biopsies were obtained and sent to pathology for evaluation.
Questions:
-
List 5 causes of inflamed bowel.
-
What is the most likely diagnosis in this case?
-
What are the common complications of this disease?
How to participate
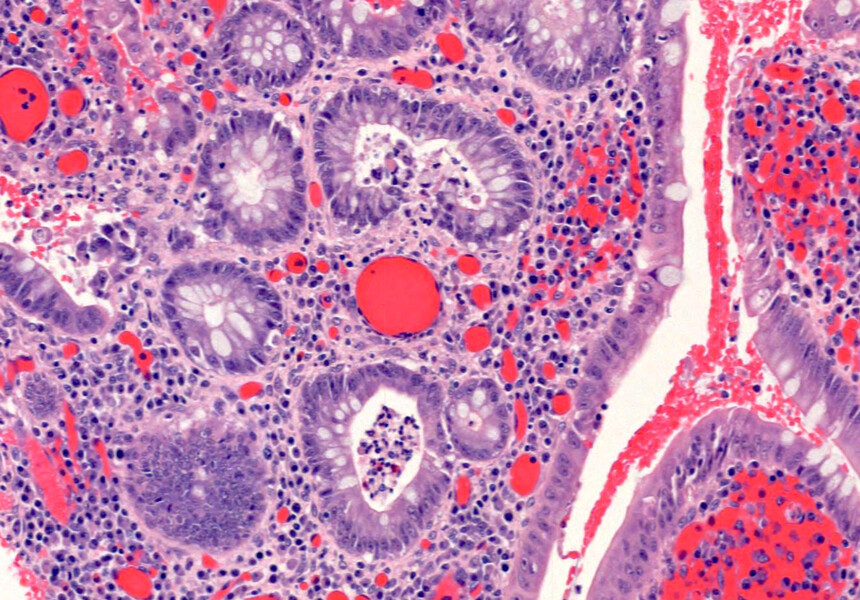
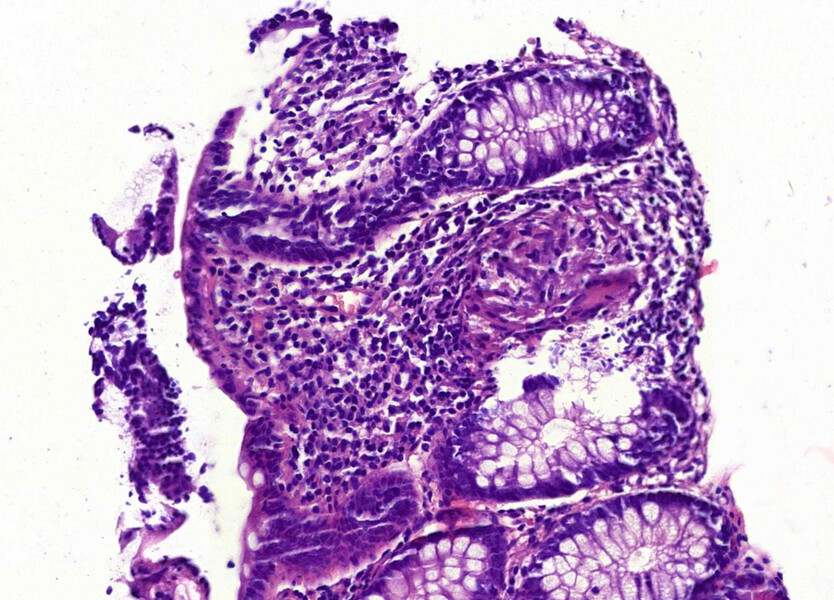
Take a look at the images.
Anyone is welcome to try to solve the puzzle by commenting on the related post on our Instagram.
If you are a medical student at the University of Toronto, you can also:
If you do, you are in for a chance to win a $100 gift card! (UofT Med students only).
Discover the answer to April's Case of the Month challenge!
The answer to April’s Case of the Month is Crohn’s disease!
Causes of inflammation in the gastrointestinal tract include infection, autoimmune diseases including inflammatory bowel disease, drugs, ischemia, and diverticulitis.
Crohn’s disease is a type inflammatory bowel disease. Ulcerative colitis is another type of inflammatory bowel disease. Both are chronic autoimmune conditions that cause inflammation in some parts of the gastrointestinal tract. Crohn’s disease typically involves the colon and terminal ileum with a patchy distribution, while ulcerative colitis involves the colon in a contiguous fashion starting at the rectum. On biopsy, both conditions can show active inflammation (such as neutrophils infiltrating the epithelium, crypt abscesses, and ulceration). Chronic inflammation causes changes in the histological architecture of the bowel. Granulomas may be seen in Crohn’s disease, but typically not in ulcerative colitis. Crohn’s disease often involves the whole thickness of the bowel wall, while ulcerative colitis typically only involves the mucosa. Malabsorption, malnutrition, strictures, and fistula are common complications of Crohn’s disease.
If you are a current medical student at U of T, you can register to join the April case of the month lecture online or in person and have a chance to win a $100 gift card!
You can also join the Special Interest Group in Laboratory Medicine to learn more about Laboratory Medicine.
Laboratory Medicine and the study of disease for medical students

