Main Second Level Navigation
Nov 22, 2022
Clinical Embryology graduate presents research at CFAS conference
Programs: Graduate, Programs: MHSc Lab Medicine, Agile education, Impactful research, Dynamic Collaboration
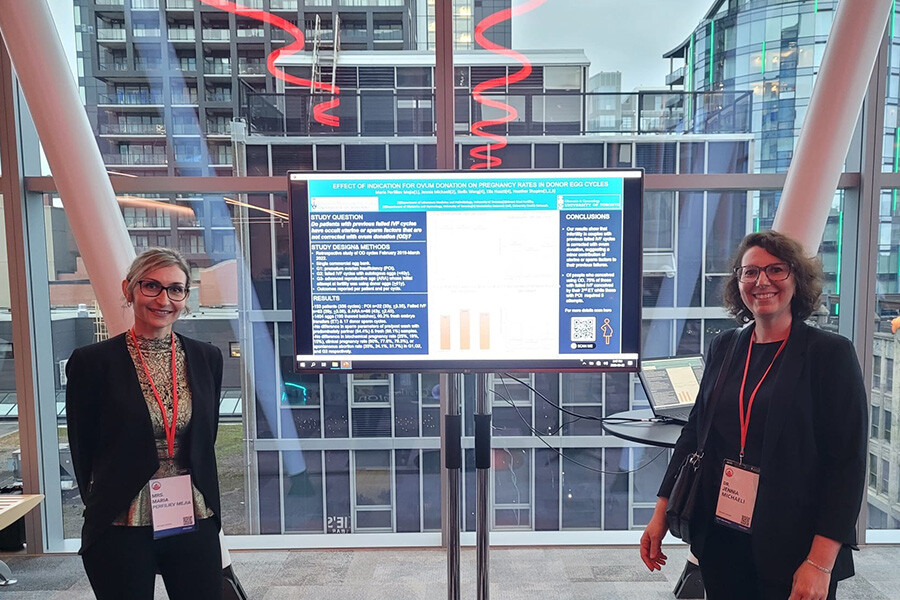
Maria Perfiliev Mejia (left) presenting her Capstone project results with Dr. Jennia Michaeli, OBGyn REI Fellow (Reproductive Endocrinology & Infertility)