Pathologists' Assistant Bootcamp: a collaborative effort across Toronto hospitals

Dr. Klaudia Nowak was fresh out of her fellowship and a new faculty member in the Department of Laboratory Medicine and Pathobiology in the Temerty Faculty of Medicine when she was asked to help train Pathologists’ Assistants (PAs). Dr. George Yousef, Medical Director of the MHSc in Laboratory Medicine asked her to bridge the gap between the Masters’ program didactic learning in first year, and hands-on practical rotations in hospitals in the second year.
She teamed up with Pathologists’ Assistant Will Tsui, and together they created the PA Bootcamp which we dissect in detail in this case study.

The problem: getting PAs ready for the lab
Pathologists’ Assistants are a vital part of the pathology laboratory. They are the first to receive specimens and do the initial ‘gross’ examination. They prepare the samples and ultimately decide what the Pathologist looks at to make their diagnosis.
Students in the MHSc in Laboratory Medicine, Pathologists’ Assistant Field learn theory in their first year and spend most of their second year rotating through hospital sites, so needed to adapt from classroom to gross room.
Not only did Nowak and Tsui need to make sure the PAs were confident to step into a gross room, but that they were ready to experience rotations across multiple sites when every hospital runs their labs differently and approach samples in different ways.
The solution was to create a huge collaborative effort across Toronto that exposed students to the many different approaches and unique perspectives of multiple hospitals. Added to this challenge was the program launching in September 2020 during the COVID-19 pandemic, so some elements needed to be online, but able to switch to in-person when possible.
Creating a curriculum: bridging theory to practical
Irina Shipilova, PA at SickKids (now at Joseph Brant Hospital, her role now taken by Emmanuelle Chung at UHN) joined the team comprised of Nowak, Gastrointestinal (GI) Pathologist at Toronto General Hospital, and Tsui, PA at Mount Sinai. Emily Almeida (Mount Sinai, now in New Zealand) and Farhana Harji (St. Mike’s) joined at the same time as Emmanuelle.
They were allocated two weeks at the start of May and wanted to base it on Dr. Susan Lester’s Manual of Surgical Pathology. They decided to design the curriculum around three main components:
1. Didactic series
Students would begin their day in a lecture where they are shown a particular sample and how to examine and dissect it.
Around 30 Pathologists’ Assistants take part in presenting the lectures, alongside one Medical Laboratory Technician (MLT) and one Pathologist (Nowak). It was important to the team to have representation from across all the hospital sites involved in the second-year practicums and to be all inclusive.
Managing the large number of lecturers was easier when teaching online (using Articulate 360) during the COVID-19 pandemic, but engagement from the students was lower. Now with teaching in person, PAs travel from all over the Toronto area to deliver their lectures.
Not only was their aim to teach the students, but to show the diversity of the profession and its importance. PAs were given guidance for their lectures and all materials were screened by the lead team. The lectures gave students a breadth of insight into the different perspectives and ways of working at each hospital.
2. Putting didactic learning into practice
After the lecture, students have a hands-on session where they practice what they learned in the morning. Rotating through three sites during the Bootcamp: UHN, St. Michael’s Hospital (Unity Health) and Mount Sinai, one challenge was ensuring access to samples that had been covered in the morning lecture, which wasn’t always possible.
This year, the Bootcamp is focussing mainly on various types of biopsies and small resections like gallbladders and appendices, based on student feedback.
3. Tours of hospital sites
Another main component of the Bootcamp is exploring some of the spaces associated with their future profession. They receive tours of histology labs, autopsy rooms, and join the Gross Rounds run by Dr. Carlo Hojilla at Mount Sinai and online Autopsy Rounds run by Dr. Michael Seidman at Toronto General Hospital.
Other learning opportunities
In addition to the three main components, the students also complete some time on frozen sections. Usually, samples are treated and embedded in wax and then thinly sliced so they can be viewed under the microscope, a process that can take up to 24 hours. When specimens need to be examined more urgently, they are frozen and sectioned.
They also receive career experience and advice through a panel discussion in their second week. PAs at various stages of their careers come in to talk to the students and answer any questions they may have. This allows them to network and build community, see what trajectories they can take and what else they can do outside the gross room.
Although it was accepted that each hospital has its own unique approach, standardisation is an important part of the curriculum development. For example, the approach to teaching frozen sections in St. Michael’s and Mount Sinai was so different that MLT Malek Hamdani developed guidelines on how to present the frozen sections to students for all hospital sites after student feedback.
Assessment and feedback
The Bootcamp utilises multiple methods of assessment and feedback. It was equally important to assess the students, and to gather feedback to develop the course.
Methods used include:
- Pre-test and Post-test: students complete the same multiple-choice assessment at the start and end of Bootcamp. These figures showed that students’ knowledge increased by at least 30% over the two weeks.
- Lecture feedback: QR codes were shown at the end of each lecture so students could quickly and easily complete a short evaluation. Although resulting in approximately 150 responses for the team to assess, it gives them valuable insights into developing the course.
- Practicum assessment: Preceptors give feedback to the students on how well they performed in the practical elements and students give feedback on how they thought the practicum went and how comfortable they feel about performing it.
- Townhall-like discussions: after their career panel they hold a Q&A session and discuss what everyone thought of the PA bootcamp.
- Ensuring a welcoming learning environment: one question asked at the end of the Bootcamp is whether students thought it was a safe professional learning environment. It is paramount to the team that students are not afraid to ask questions or make mistakes because the point of the bootcamp is to learn, not judge.
A cross-institutional collaborative effort
Although there are only five students in the PA program each year, they are taught by over 40 professionals across Toronto which is a huge collaborative effort.
Not only does this provide a unique learning opportunity for the students and prepare them for a career of excellence, but it exposes them to the variability and different perspectives between sites.
The program itself, shines a light on the profession and the deep collegiality and interdepartmental relationships between hospital sites and the University of Toronto.
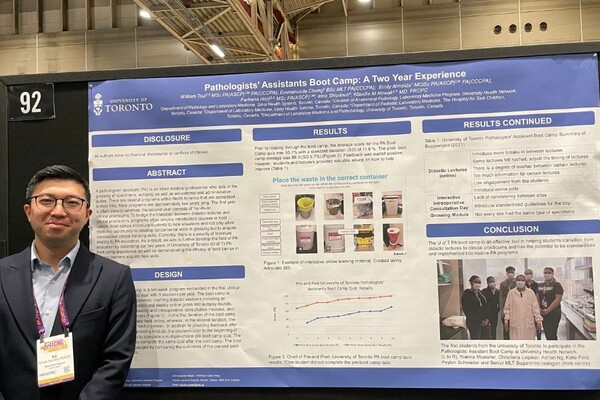
The PA Bootcamp team, now also including Katie Greenall (Sunnybrook) and Keeley Burnside (SickKids), recently presented the PA Bootcamp as a blueprint for all PA training programs across Canada at this years USCAP (United States and Canadian Academy of Pathology) meeting.
Find out more
The MHSc in Laboratory Medicine
Faculty profiles for Klaudia Nowak and Will Tsui
See also from UHN News: Preparing pathologists' assistants for the gross room
Meet Pathologists' Assistants in our Humans of LMP Q&As:
The LMP Strategic Plan 2023 - 2028




